Information for Policymakers
Shoring up access to midwifery is a critically important solution to reversing our maternal health crisis and the precipitous decline in access to maternal care across the state.
DOWNLOAD THE PACKET which includes a summary page & fact sheets for each of the midwifery and birth center bills.
(Not a policymaker? Learn more and join the movement for access to midwives in Massachusetts.)
Midwives Save Lives
The maternal health crisis is an emergency and urgent action is needed.
Midwives are a solution, but Massachusetts lags.
The Massachusetts state legislature took an important step in the FY24 budget which provided grants to open new non-profit birth centers like Neighborhood Birth Center, funding for the Seven Sisters Birth Center, and investments to reopen Cambridge Birth Center. However, policy barriers including outdated state regulations and inequitable reimbursement continue to stifle birth center options in the Commonwealth.
Massachusetts can leapfrog from lagging to leading on midwives and birth centers by enacting key legislation.
Bills
Pending legislation that will integrate midwifery care, expand access, enable birth centers to thrive, and increase birth options:
H.2209/S.1457, An Act promoting access to midwifery care and out-of-hospital birth options, sponsored by Sen. Becca Rausch, Rep. Kay Khan, and Rep. Brandy Fluker Oakley, creates a pathway to licensure for certified professional midwives and make their care reimbursable by Medicaid/MassHealth.
DOWNLOAD THE FACT SHEET ON MIDWIFERY AND OUT-OF-HOSPITAL BIRTH
H.3616/S.1335, An Act updating the regulations governing licensed birth centers in Massachusetts, sponsored by Sen. Jo Comerford, Rep. Manny Cruz, and Rep. Chynah Tyler, addresses onerous and outdated birth center regulations.
DOWNLOAD THE FACT SHEET ON BIRTH CENTER REGULATIONS
H.1069/S.607, An Act to Increase Access to Nurse-Midwifery Services, sponsored by Rep. Kay Khan and Sen. Brendan Crighton, ensures insurance reimbursement parity for certified nurse midwives.
DOWNLOAD THE FACT SHEET ON NURSE-MIDWIFERY REIMBURSEMENT
S.1415, An Act relative to birthing justice in the Commonwealth, sponsored by Sen. Liz Miranda, includes language from the above-referenced midwifery and birth center bills as well as additional urgently-needed policies for optimal maternity care and to address longstanding racial inequities.
Funding: In addition to legislation, we need sustained investment to expand birth centers and the midwifery workforce.
These policies will implement the recommendations of the Commission on Racial Inequities in Maternal Health and the Health Policy Commission to address rising maternal mortality and morbidity, reduce racial inequities, and lower health care costs.
Update 11/15/2023 — The Healey Driscoll Administration is taking steps to address gaps in maternal health care including updating birth center regulations and equitable MassHealth reimbursement for midwifery services. We applaud these steps and urge for legislation to complement the actions being undertaken by EOHHS. Read more.
select recent media coverage
Commonwealth Magazine “Hoping to deliver at a Massachusetts birth center? Good luck. Planned closure of North Shore facility will leave just one birthing center in the state.” by Shira Schoenberg (Nov 20, 2022)
Boston Globe “‘Another assault on women’s rights’: Last birth center in Eastern Massachusetts to close. The cuts come as lawmakers killed proposals linked to improved maternal care for people of color.” by Kay Lazar (June 13, 2022)
MassLive “Home birthing options limited due to lack of midwife licensing; This bill could change that.” by Alison Kuznitz (March 28, 2023)
Boston Globe “Editorial: License midwives to help struggling birth centers.” (March 5, 2023)
Commonwealth Magazine “Opinion: Take pregnant people seriously, support birth centers. Let science in to address failing maternity system.” by Cristina Alonso (Jan 1, 2023)
What is a Midwife?
A midwife is a clinical health care provider with a low-tech, high-touch approach. Midwives view pregnancy and birth as normal life events and their approach centers on physiologic birth, holistic care, and informed consent. There is a large body of evidence, including the federal Strong Start study, that have shown a clear and significant benefit with midwifery care — better health outcomes, better patient experience, and lower health care costs.
What is the difference between a midwife and a doula? Midwives provide clinical health care for both the birthing person and baby. Doulas offer physical, emotional, and informational support for the birthing person —not clinical care.
What types of midwives work in Massachusetts?
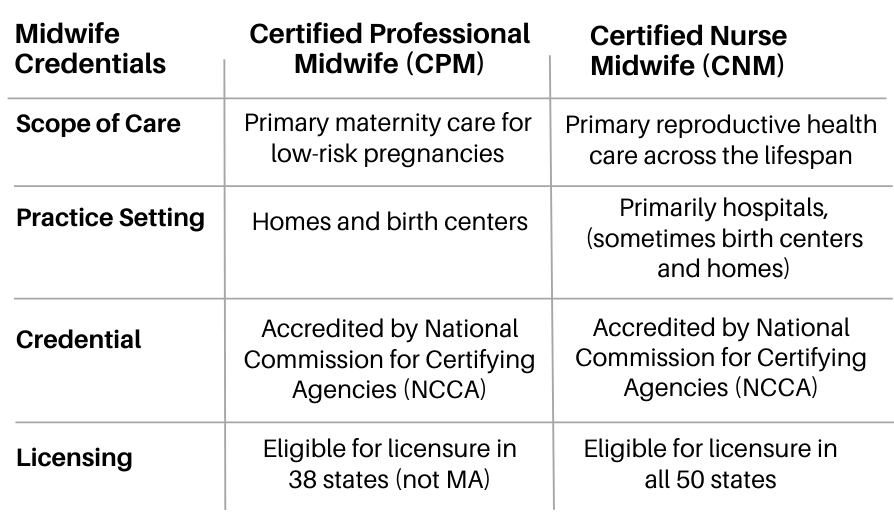
Certified Professional Midwives (CPMs) and Certified Nurse Midwives (CNMs) both practice in Massachusetts, though our state ranks poorly on midwifery integration when compared to other US states. We are one of just a dozen states that does not yet integrate CPMs into the health care system, meaning their are ineligible to get a state license, to practice in a birth center, or to get insurance and MassHealth reimbursement. We are also lagging when it comes to appropriate reimbursement for midwifery care and updated regulations to facilitate the safe and sustainable operation of birth centers.
The table below provides an overview of the two predominant midwifery credentials in Massachusetts:
Why we need policy action on midwifery
Earlier this year in Time Magazine, former heads of Health and Human Services Tommy Thompson and Kathleen Sebelius described our nation’s maternal health care system as “failing parents and their babies.” They urged policymakers to leverage the powerful benefits of midwifery care. Our maternal health crisis is preventable and urgent. The good news is: we know what works! Midwives are the norm in wealthy countries with much lower maternal mortality than ours.
Bay State Birth Coalition is a consumer advocacy group dedicated to expanding access to midwifery care in Massachusetts. Midwifery care is a key opportunity for system improvement in Massachusetts. The Commission on Racial Inequities in Maternal Health has recognized integrating and expanding access to midwives as an essential tool to improve maternal health outcomes and reduce racial inequities. Unfortunately, Massachusetts has fallen way behind other states for integrating midwives into the health care system, ranking 32nd in a 2018 study (and we have only fallen further behind since).
Our communities have been losing access to maternity care and midwifery as health care systems and provider practices close and consolidate. In just the past 6 years, hospitals have closed maternity wards, eliminated midwifery care, or shuttered birth centers in Taunton, Wareham, Cambridge, Falmouth, Holyoke, Beverly, and Leominster. Though there are now 400 freestanding birth centers providing midwife-led care across the US, Massachusetts has only 1 (Seven Sisters in Northampton) while New Hampshire has 4, Maine has 3, California has 56, and Texas has 92. Increased utilization of midwives would help reverse the trend of diminishing access, declining options, and worsening maternal and infant health outcomes in Massachusetts.
People in Massachusetts have also shown that we want midwifery care:
Families have been protesting and rallying in response to closures of birth centers in their communities.
The rate of midwife-attended home births has skyrocketed, rising by 47% since 2019.
The only freestanding birth center operating in the state, Seven Sisters Midwifery in Northampton, has had to hire more midwives to meet the tremendous demand since they opened in 2020, including families traveling from hours away.
Other families are driving to New Hampshire birth centers.
Birthing people and their babies survive and thrive under midwives’ holistic model of care and their reduced use of unnecessary and expensive medical intervention for low risk pregnancies. It has been shown in numerous studies over decades that access to midwives reduces deaths, reduces C-sections, and increases breastfeeding rates while lowering health care costs. A recent study by the Massachusetts Health Policy Commission found the same.
Importantly, midwifery centers the birthing person and their bodily autonomy, and gives us a choice of where we’d like to give birth (hospital, home, or birth center). We emerge from our births feeling strong, healthy, and empowered.
Communities across the Commonwealth are being denied access to midwives, to a choice about where we give birth, and to the model of care we want. We should be leading the way in utilizing the midwifery workforce to improve outcomes and access to care. Let’s not keep watching other states pass us by.
Evidence and research Highlights
Commonwealth Fund: “How Expanding the Role of Midwives in U.S. Health Care Could Help Address the Maternal Health Crisis” (May 5, 2023)
Maternal Mortality, Severe Morbidity, and Racial Inequities rise
Maternal mortality in the U.S. has doubled in the last 20 years. “Maternal death rates have consistently been the highest among Black women, and those high rates more than doubled over the last twenty years. For Native American and Alaska Native people, the rates have tripled.” (NPR, “U.S. maternal deaths keep rising. Here's who is most at risk,” July 4, 2023)
Severe Maternal Morbidity has doubled in Massachusetts over 10 years. The Department of Public Health released a new report which details horrifying data about birthing people who nearly died or suffered grave injury, termed “severe maternal morbidity.” The report breaks down the data by race, disability, and other social and health factors to uncover the impact of racism and ableism on maternal health care. The report also points to the recommendations of the Commission on Racial Inequities in Maternal Health to address the problem. (Massachusetts Department of Public Health, Data Brief: An Assessment of Severe Maternal Morbidity in Massachusetts: 2011-2020, Released: July 2023)
Roadmap to Equitable Care and Improved Outcomes includes Midwifery and Out-of-Hospital Birth
In 2022, the Massachusetts Special Legislative Commission on Racial Inequities in Maternal Health released a comprehensive report, the result of a year of work by the Commission including listening sessions around the state. The report details the deficiencies in our maternal health care system, the impact of structural racism on maternal health, and the necessary remedies. The Commission recommended passing legislation to license CPMs, allow MassHealth to reimburse CPMs, ensure equitable access to home birth, improve reimbursement rates for nurse midwives, and scale up freestanding birth centers. (Commission report)
In 2021, the Massachusetts Health Policy Commission found a 10% in midwife- attended births would result in: 3560 fewer cesarean births, 860 fewer episiotomies, and $530 saved per birth. The HPC recommended increasing rate of midwifery care and removing barriers to opening and operating freestanding birth centers. (HPC report on midwives)
Demand for Out-of-Hospital Birth Skyrockets
Home birth rate at highest level in 30 years. The most recent data from CDC show that the home birth rate has risen steeply since 2019 to the highest level in 30 years, with the steepest increases among Black and Latinx birthing people. In 2020, Massachusetts had the fifth-highest increase in home births (47%) compared with other states and this elevated demand held for 2021 and 2022.
More Studies Finds Midwifery Safe
"Our findings show that when a state has systems to support the integration of community midwives into the healthcare system as Washington has done, birth centers and homes are both safe settings for birth. Washington provides a model for midwifery care and safe community birth that could be replicated throughout the U.S.," said Nethery, the study’s author. "Currently, some U.S. states currently have no licensure available for community birth midwives at all, and this could be contributing to poorer birth outcomes in those states."
University of British Columbia study, "Planned home birth presents little risk where midwifery is well-integrated." ScienceDaily. ScienceDaily, 7 October 2021.
Elizabeth Nethery, Laura Schummers, Audrey Levine, Aaron B. Caughey, Vivienne Souter, Wendy Gordon. “Birth Outcomes for Planned Home and Licensed Freestanding Birth Center Births in Washington State.” Obstetrics & Gynecology, 2021
Integrating Midwifery Lowers Health Care Costs
“Each shift of one percent of births from hospitals to homes would represent an annual cost savings to society of at least $321M” per the most recent of numerous studies demonstrating the cost savings associated with midwifery care.
“This study provides an estimate of the average cost of a midwife-assisted home birth in the United States. We also estimate the potential collective savings for families, insurers, and taxpayers from an increase in out-of-hospital births. Federal and state governments must decide whether to lift restrictions on midwives, while public and private insurers face the question of whether to cover home births. There are more than 3.6 million births every year in the United States. With the cost of birth spread across public assistance programs, employer-funded insurers, family-funded insurers, and families paying out-of-pocket, the 65.7% lower cost of home births relative to hospital births represents an opportunity for substantial savings for governments, employers, insurance providers, and households. Changes in legislation, corporate policies, and attitudes regarding out-of-hospital births could reduce the health care burden in the United States by several billion dollars annually.” (Cost study)